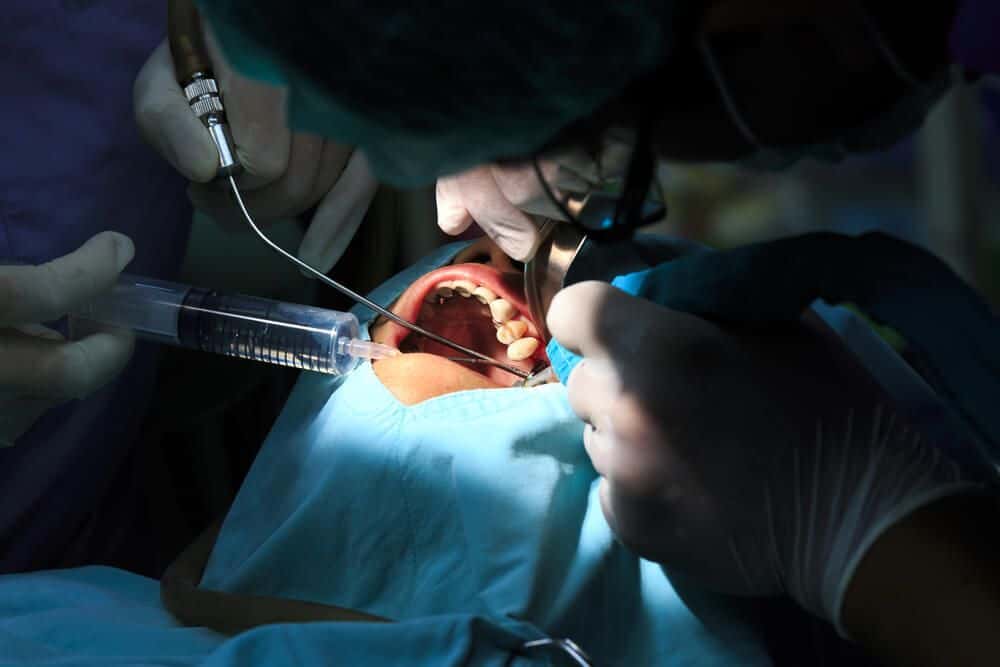
Failure to Administer Antibiotics After Tooth Extraction Leads to Infection
This special care dentistry case takes place in Nevada and involves a male patient who had a long history of extremely poor dental hygiene.
Updated on
As a result of this long history of poor hygiene, the patient required extensive dental care, including the removal of several teeth. After undergoing his first extraction, the dentist noted that the tooth and socket appeared relatively healthy and free of infection. A few days after the procedure, the patient returned to the dentist complaining of severe pain in the socket of the extracted tooth. The dentist noted no abnormalities during this visit, and sent the patient home with instructions to follow up should the pain become worse.
Several days later, the patient again returned to the dentist complaining of even worse pain; it was at this point that the dentist began to administer antibiotics. The next day, the patient began to vomit uncontrollably, and was unable to consume any solid food or liquids. Several hours after the vomiting began, the patient also began to experience muscle spasms that prevented him from opening his mouth.
The patient returned to his dentist emergently, who immediately told him to go to the emergency room. The patient was given a range of antibiotics over the next few weeks, however they proved ineffective and he was eventually admitted to the hospital. There, it was discovered that the patient’s infection had penetrated the bone in his jaw, and surgery was performed to remove the infected tissue and bone. It is alleged that the Plaintiff should have received antibiotics immediately after the extraction due to his poor oral health, and that the infection that resulted could have been prevented with proper care by the extracting dentist.
Question(s) For Expert Witness
1. Based off of the case summary do you believe that the dentist may have acted below the standard level of care when he did not prescribe antibiotics immediately after the tooth removal even though he had an extensive history of poor dental hygiene?
Expert Witness Response E-000943
 The indications for antibiotic administration for third molar removal are impaction, pericoronitis, swelling, trismus, lymphadenopathy, and fever. If the patient had any of these, antibiotic administration was indicated. If the patient states any of these were present, then there may be a question of fact over the dentist's testimony. Poor oral hygiene and smoking do not in themselves justify antibiotic administration. Referral to a physician for a dental infection is inappropriate. The primary specialist competent to treat dental infections is the oral and maxillofacial surgeon (OMS). Likely, if the dentist had referred this patient to an OMS, the infection would have been treated much more rapidly, effectively, and with less invasive surgery. Sometimes a general dentist will not refer a postoperative infection to an OMS out of embarrassment at not having referred the case to an OMS in the first place. Inappropriate referral is the likely breach of the standard of care here, with possibly failure to prescribe an antibiotic in the conditions described above.
The indications for antibiotic administration for third molar removal are impaction, pericoronitis, swelling, trismus, lymphadenopathy, and fever. If the patient had any of these, antibiotic administration was indicated. If the patient states any of these were present, then there may be a question of fact over the dentist's testimony. Poor oral hygiene and smoking do not in themselves justify antibiotic administration. Referral to a physician for a dental infection is inappropriate. The primary specialist competent to treat dental infections is the oral and maxillofacial surgeon (OMS). Likely, if the dentist had referred this patient to an OMS, the infection would have been treated much more rapidly, effectively, and with less invasive surgery. Sometimes a general dentist will not refer a postoperative infection to an OMS out of embarrassment at not having referred the case to an OMS in the first place. Inappropriate referral is the likely breach of the standard of care here, with possibly failure to prescribe an antibiotic in the conditions described above.
About the author
Joseph O'Neill
Joe has extensive experience in online journalism and technical writing across a range of legal topics, including personal injury, meidcal malpractice, mass torts, consumer litigation, commercial litigation, and more. Joe spent close to six years working at Expert Institute, finishing up his role here as Director of Marketing. He has considerable knowledge across an array of legal topics pertaining to expert witnesses. Currently, Joe servces as Owner and Demand Generation Consultant at LightSail Consulting.
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.
Sign up nowFind an expert witness near you
What State is your case in?
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.